The organ donation process is carefully regulated for patient safety and conducted with the utmost respect for donors and their families. Organ procurement organizations (OPO) such as Gift of Life Michigan must adhere to medical, ethical and legal standards.
Brain death is death. Physicians at hospitals across the nation make the determination, or declaration, that a patient has died before that individual can become an organ donor. It’s important to understand what brain death is and how it’s determined in this context.
What is brain death?
De acuerdo con la American Academy of Neurology, brain death is the irreversible and complete loss of brain and brain stem function. It is both a legal and medical definition of death.
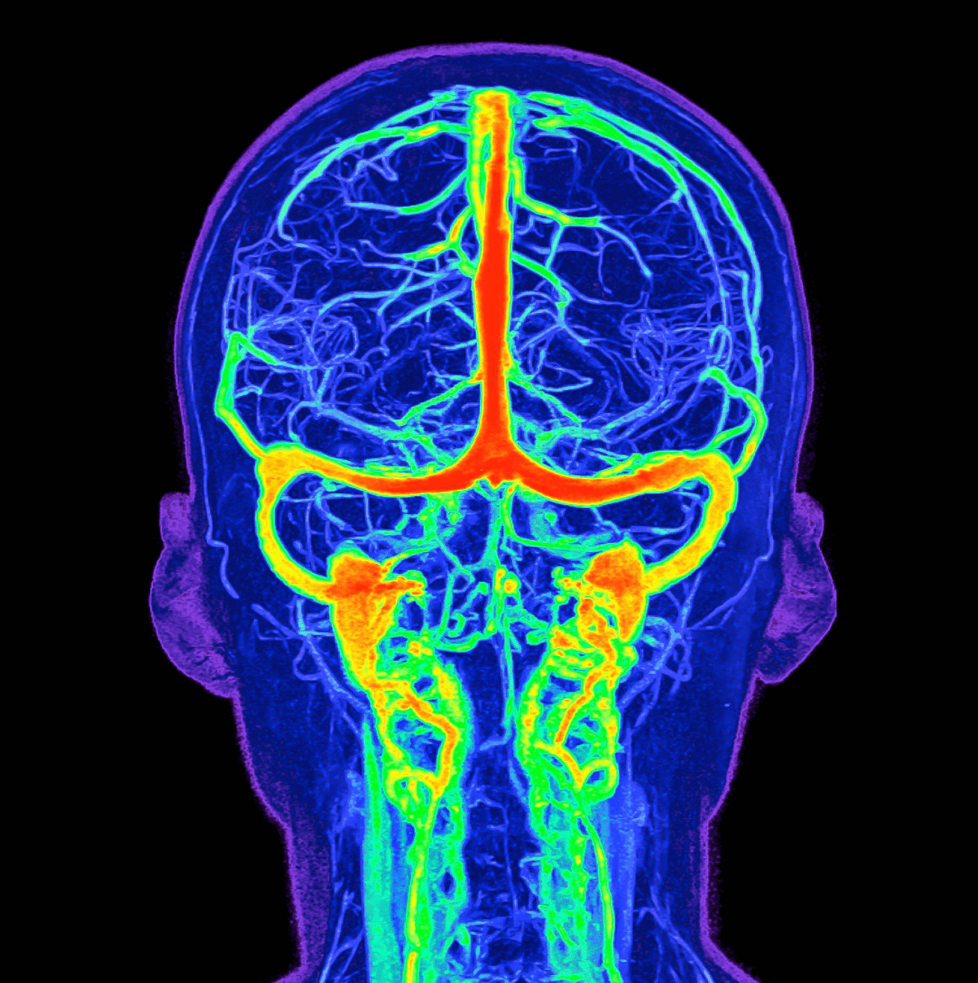
Brain death typically occurs after a major injury or illness where the blood supply to the brain is blocked, or the brain begins to swell within the skull. This can take place after a traumatic head injury, a stroke or if the heart stops for a prolonged period. These traumatic events cause the brain to lose oxygen or begin to swell beyond recovery.
Brain death is not the same as a coma or a prolonged vegetative state. The latter two are medical states where the patient may be unconscious but still show brain function. There is no brain function in brain death.
Who determines brain death?
As an OPO, Gift of Life is not involved, nor has any say, in the declaration of brain death.
Brain death is determined by strict medical and legal criteria. A patient must undergo extensive testing and verifications before they are declared brain dead by a physician.
A patient is not evaluated for organ donation or brain death until hospital teams have attempted all life-saving measures. The hospital staff working to save the patient’s life is entirely separate from the teams that evaluate patients for organ donation potential and the transplant teams.
It’s often difficult for families to understand brain death because the patient is on a ventilator, which maintains breathing and organ function. The ventilator keeps blood and oxygen flowing to their organs. Their heart continues to beat, and their skin remains warm.
Once a physician declares a patient deceased, Gift of Life coordinates with transplant teams to recover organs. The patient is carefully screened for donation eligibility. We work closely with the patient’s family to honor their loved one’s decision if they are a registered donor. If the patient isn’t registered, Gift of Life asks the family if they would like to authorize donation on their behalf.
FAQs of brain death
Is brain death common?
No, it’s not. One analysis found that in the U.S., brain deaths accounted for just 2% of all hospital deaths involving adults.
What is the main cause of brain death?
Many things may cause severe, permanent brain damage that leads to brain death. For example, the brain needs blood and oxygen to function, so any serious injury or illness that keeps blood and oxygen from the brain may cause brain death. Likewise, any injury or illness that damages blood vessels in the brain and causes bleeding may lead to it.
Potential causes
- Traumatic brain injury
- Intracerebral hemorrhage (brain bleed)
- Subarachnoid hemorrhage (bleeding between the brain and cranium)
- Ischemic stroke (blood clot or injury blocks blood flow to the brain)
- Heart attack
- Hypoxic ischemic brain injury (brain doesn’t get oxygen)
- Intracranial infections (meningitis or encephalitis)
What tests are done to determine brain death?
Healthcare providers with special training in brain death do several tests. They may do tests more than once to confirm their initial diagnosis. If a provider suspects brain death, they’ll tell the patient’s family about the tests and what the tests might show. Tests include a physical examination, imaging of the brain, an extensive neurological examination and an apnea test to determine if the patient can breathe on their own.
Neurological examination
In brain death, patients don’t react to noise, lights or touch as they would before a brain injury. They may move, but the movement is involuntary, meaning they didn’t move on purpose. Providers doing a neurological examination to diagnose brain death will:
- Check the gag or choking reflex by touching the back of the throat.
- Check eye reflexes by touching an eye with a cotton swab to see if the patient flinches, blinks, closes their eye or moves their head.
- Check the pupils’ response to light.
Apnea test
If the patient has a catastrophic brain injury, they can’t breathe on their own and rely on ventilators. In an apnea test, providers briefly stop ventilator support to see if the patient takes a breath on their own.