Advances in technology and continued expansion of the Organ Donor Registry helped Gift of Life Michigan – and organ procurement organizations across the country – save more lives than ever in 2019.
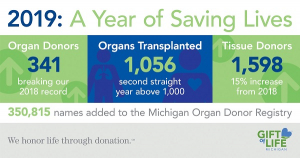
In Michigan, 341 patients donated organs and 1,598 donated tissue last year. Both are increases from 2018 and signify the sixth consecutive year of increased donation. In total, 1,056 organs were transplanted.
Across the country, the transplantation field saw some technological advances designed to help improve the odds of successful donation and transplantation.
In early December, doctors at Duke University Hospital performed the first-ever adult heart transplant through donation after circulatory death (DCD) here in the U.S. There have been a handful of successful procedures since then, but the new process could have dramatic implications on the number of heart transplants that take place each year.
Typically, heart transplants depend on a declaration of brain death, when a patient is stabilized with a ventilator. DCD transplants, on the other hand, occur after circulatory death. They rely on hearts that have stopped beating, when the patients have no chance of recovery.
Duke surgeons used a TransMedics Organ Care System, a warm perfusion pump approved by the FDA for clinical trials at five medical centers to help keep the organ viable. The implications are impressive: the ability to perform DCD heart transplants could increase the donor pool by as much as 30 percent, providing hope to thousands of patients on the transplant waiting list.
Innovation of these and other types of pumps will help improve the odds of successful transplantation. They are built on the premise that organs do not need to be cooled in order to be transplanted successfully and they are being used more frequently. A number of transplant centers, including a couple of Michigan centers, are now using normo-thermic and/or hypothermic devices to improve and extend the time between organ recovery and implantation. Henry Ford Health Systems, for example, uses the TransMedic device for donated livers. The device has shown to improve the viability of livers previously deemed unsuitable for transplantation. Similarly, the University of Michigan uses the OrganOx normothermic device for livers.
Likewise, advancements in external lung pumps have helped make some previously non-viable lungs suitable for transplantation.
Performing successful organ transplants is a complex equation involving time, distance and biological compatibility. At Gift of Life Michigan, we are continually working to solve that equation and improve results to save and enhance as many lives as possible. We’re looking forward to 2020, and the new hope it will bring to thousands of people awaiting these life-changing procedures.